The Partner: Vermont Child Psychiatry Access Program (VTCPAP)
VTCPAP’s team of licensed clinical social workers and board-certified child and adolescent psychiatrists provide education and tele-health consultation to primary care providers (PCPs) who, in turn, provide care to their pediatric or maternal patients in need of mental and behavioral health treatment.
Trayt Health’s Access Portal is central to VTCPAP, supporting and enhancing clinician workflows, streamlining and coordinating program activity and care, and capturing patient and program outcomes with robust reporting and insights.
The Challenge
Between 2018 and 2021, Vermont saw a 60% increase in children aged 3 to 8 years old with a mental, emotional or behavioral health condition. As with many states, it also faced an acute lack of providers, with multiple counties lacking a single child and adolescent psychiatrist. These shortages leave the primary care setting as many patients’ only avenue for mental health care, straining community resources and expertise in the absence of specialist psychiatric care.
The Solution: Empowering Primary Care Physicians at the Point of Care
In response to this escalating mental health crisis, child and adolescent psychiatrist Dr. Greta Spottswood was part of a state collaborative that formed the Vermont Child Psychiatry Access Program (VTCPAP). Launched in June 2022, VTCAP’s mission is to equip primary care providers (PCPs) with the tools and resources needed to address these pressing concerns. As Dr. Spottswood saw it, “Being on the ground in primary care made me want to figure out a way to support more PCPs across Vermont and I was inspired by how Access Programs were improving care in other states.”
As one of roughly 50 Child Psychiatry Access Programs (CPAPs) across the nation, VTCPAP bridges gaps in care access by connecting PCPs across the state with child and adolescent psychiatrists and licensed social workers for telephone consultation, referral support, training and education. Through financial support from a range of federal, state and private sources, Access Programs expand the impact of specialty care while equipping PCPs with the knowledge and skills to deliver specialty-level care in the future.
“Trayt was unique in scope and underlying organizational values. We’ve been able to seamlessly collaborate with Trayt in both the daily work of answering calls to PCPs, and also some sophisticated analysis around the content and impact of our conversations with PCPs.”
— Dr. Greta Spottswood, VTCPAP Medical Program Director
Access through technology: VTCPAP and Trayt Health
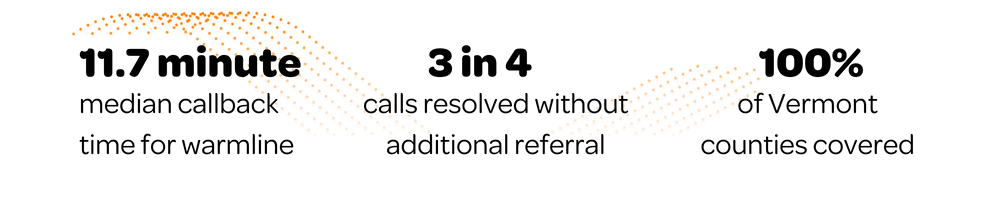
To fully realize the vision of VTCPAP, program leadership needed a behavioral health tech platform that could facilitate collaboration and care measurement. As the partner to CPAPs in Vermont, Nebraska and Texas, Trayt Health has crafted its tailored data analytics and clinical workflow Access Portal to serve as the technological backbone for CPAPs and perinatal psychiatry access programs, enabling them to serve and scale. Trayt’s platform facilitates easy enrollment of clinics and physicians while providing valuable insights for program optimization. Trayt’s real-time clinician dashboard has significantly reduced VTCPAP callback times to a median of 11.7 minutes, ensuring timely and equitable consultations.
This speed means the PCP can often speak with a specialist while a family or child is still in the clinic, ensuring continuity and clarity of care. Trayt’s insights offer visibility into how VTCPAP delivers on its goal of equitable access: 20% of consults are delivered to behavioral health deserts (counties with no registered child and adolescent psychiatrists) – as well as effectiveness – 3 in 4 consults were resolved without requiring additional referral and nearly 9 in 10 consults were resolved without requiring additional consultation. Trayt also allows VTCPAP hub staff to quickly and easily enroll clinics and physicians into the program, increasing engagement and the program’s reach. And when VTCPAP shares its successes with stakeholders (including funders), Trayt’s dashboards and exports provide crucial population and program-level data to outline who the program is serving, how well it is doing, and where it can improve.
Collaborating on care for Vermont’s children
To launch VTCPAP, Dr. Spottswood and her team orchestrated a statewide effort involving the Vermont Department of Mental Health (DMH), The University of Vermont’s Medical Center, The University of Vermont’s Vermont Child Health Improvement Program (VCHIP), and other organizations, culminating in funding from the Health Resources and Services Administration’s (HRSA) Pediatric Mental Health Access Care program as well as the Four Pines Fund. Since inception, VTCPAP has supported over 880 consults1 including medication management, referral assistance, diagnosis, and assessment. Nearly 92%2 of responding PCPs would be likely or very likely to recommend the program to a colleague and nearly 90%2 of responding PCPs see a moderate or significant improvement in patient outcomes due to VTCPAP, while also reporting increased wellness themselves.
As the program continues to grow and evolve, it will continue to help make targeted educational trainings available to the PCP and community therapist workforce and plans to work with state partners to make more intensive supports available faster. VTCPAP will tap into Trayt to create capabilities that will make the program even more successful and scalable. This progress animates Dr. Spottswood and the VTCPAP team: “we’re now three years in and continue honing the most functional structure possible based on feedback from PCPs and what we’ve learned about our strengths and needs organizationally.”
“We are building a better way.”
Program data as of Sep 2023 unless otherwise noted. 1Total consults as of April 2024 2Among clinicians for whom the question was applicable